Recommendations
- Everyone in South Africa should wear cloth face-masks when in public.
- Members of the public should not use N-95 and surgical masks. These medical masks remain reserved only for healthcare workers.
- The main benefit of everyone wearing a face-mask is to reduce the amount of Coronavirus or Influenza virus being coughed up by those with the infection thereby reducing its spread through droplets. Since some persons with the Coronavirus may not have symptoms or may not know they have it, everyone should wear a face-mask.
- Handwashing and social distancing remain the most important prevention strategies for Coronavirus infection since there is little evidence at this time that face-masks protect people against getting infected with the Coronavirus.
|
Rationale for everyone to wear a face-mask to reduce Coronavirus transmission
Face-masks are routinely used by healthcare workers to prevent the nosocomial spread ofinfections in hospitals. There has been considerable debate about the utility of widespread use of face-masks in the general public to prevent the spread of the Coronavirus. 1
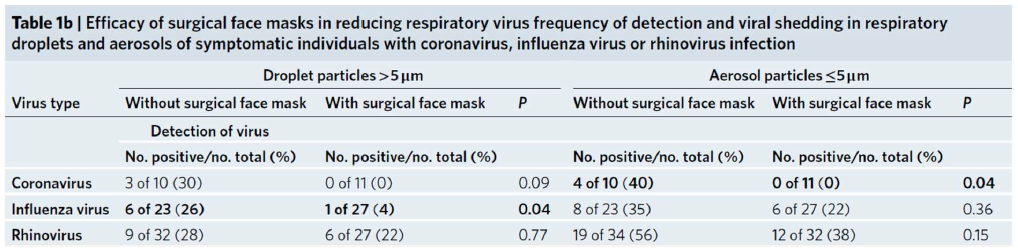
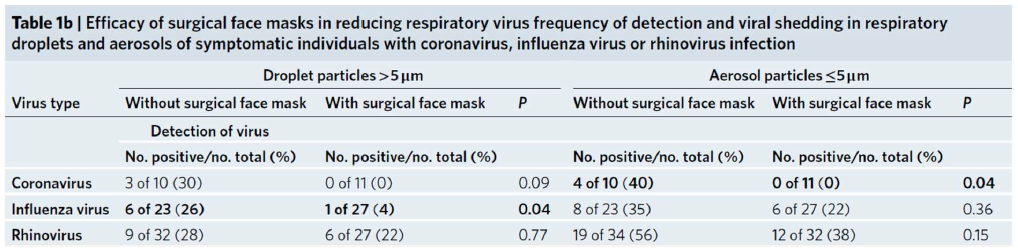
There is good evidence to show that face-masks significantly reduce the spread of infectious droplets. A recent study involving 246 patients demonstrated that face-masks significantly reduced the detection of Ccoronavirus in the exhaled breath of Covid-19 patients. While 30% to 40% of 10 patients without masks had Coronavirus in their exhaled breath, none of the 11 Covid-19 patients with masks had Coronavirus in their exhaled breath (refer to Table 1b below).2 Through lowered amounts of exhaled Coronavirus, wearing a mask should reduce the spread of virus from individuals with the virus. The masks also reduced exhaled Influenza virus, though to a lesser extent.
There is currently little scientific evidence3 to show that wearing a mask will protect people from acquiring coronavirus, which occurs mainly through contaminated hands.
In some societies, wearing face-masks is culturally accepted and commonplace, e.g. in China. While face-masks are routinely worn in South Africa, the Coronavirus pandemic requires new norms and behaviours to reduce risk. In light of recent evidence4,5 that some individuals with Coronavirus who do not have symptoms (asymptomatic) can transmit the virus to others before showing symptoms, the use of a face-mask by everyone in public settings is recommended.
Although the cloth face-mask may not be as good as a surgical face-mask in hospital settings6, the cloth face-mask is a suitable alternative to surgical face-masks for reducing droplet spread in public settings. Hence, cloth face-masks are being recommended for the general public to reduce the spread of the Coronavirus.
Note 1: Face-masks are recommended as an addition to hand-washing and social distancing – it does not replace these 2 more important prevention strategies
The cloth face-mask should never be promoted as our primary prevention strategy and should never be promoted separately from hand-washing and social distancing.
Note 2: The public should not use N-95 respirator masks and surgical masks
Surgical masks and N-95 masks are critical supplies that must be reserved for healthcare workers and other medical first responders. The public should be strongly discouraged from using these medical-use masks.
Note 3: Cloth face-masks need to be worn and cleaned properly
The face-mask must cover the nose and mouth completely. Face-masks should not be lowered when speaking, coughing or sneezing. Face-masks should not be repeatedly touched – fidgeting with the mask repeatedly is strongly discouraged as it is important to avoid touching the face with hands. The inner side of the mask should not be touched by hands. Wash hands after removing the face-mask. Wash cloth face-masks with warm soapy water and iron when dry. Each person will need to have at least 2 face-masks so that one face-mask is available when the other is being washed. If possible, iron the mask after washing as it will help with disinfection.
Author
PROFESSOR SALIM S. ABDOOL KARIM
CHAIRPERSON: MINISTERIAL ADVISORY COMMITTEE ON COVID-19
References
1 Leung CC, Lam TH, Cheng KK. Mass masking in the COVID-19 epidemic: people need guidance. Lancet. 2020; 395(10228): 945.
2 Leung NHL, Chu DKW, Shiu EYC, Chan K-H, McDevitt JJ, Hau BJP, et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nature medicine. 2020.
3 Barasheed O, Alfelali M, Mushta S, Bokhary H, Alshehri J, Attar AA, et al. Uptake and effectiveness of facemask against respiratory infections at mass gatherings: a systematic review. Int J Infect Dis. 2016; 47: 105-11.
4 Li R, Pei S, Chen B, Song Y, Zhang T, Yang W, et al. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV2). Science. 2020
5 Rothe C, Schunk M, Sothmann P, Bretzel G, Froeschl G, Wallrauch C, et al. Transmission of 2019-nCoV Infection from an Asymptomatic Contact in Germany. N Engl J Med. 2020; 382(10): 970-1.
6 MacIntyre CR, Seale H, Dung TC, Hien NT, Nga PT, Chughtai AA, et al. A cluster randomised trial of cloth masks compared with medical masks in healthcare workers. BMJ Open. 2015; 5(4): e006577.